Critical incident debriefing of registered nurses working in Emergency Medical Communication Centres
Organised debriefing is not part of the regular routine. Instead, registered nurses process their reactions on their own by acquiring more knowledge or talking to colleagues and Emergency Medical Communication Centre physicians.
Background: At Emergency Medical Communication Centres (EMCC), registered nurses deal with incidents of varying degrees of severity and different outcomes over the telephone.
Objective: To gain in-depth knowledge regarding the perceived perceptions that registered nurses need in order to handle critical incidents, and their experiences of processing such incidents afterwards.
Method: The study has a qualitative design with a grounded theory approach to obtain knowledge for developing an intervention study in the future. We conducted individual, semi-structured interviews with 6 registered nurses working at an Emergency Medical Communication Centre operated by a Norwegian regional health authority.
Results: The analysis showed that the ‘situational awareness’ of registered nurses has a bearing on how they deal with critical incidents and debrief afterwards. The registered nurses in this study chose different strategies for debriefing depending on the circumstances, including factors such as time, the provision of organised debriefing and their perception of their own needs. Registered nurses debrief primarily on their own (‘self-help’) by taking short breaks, receiving feedback from and having spontaneous discussions with colleagues, and by preparing themselves to deal with future incidents. Situations also occurred in which the registered nurses sought support in professional reviews with Emergency Medical Communication Centrephysicians who were acquainted with the situation and other personnel. Organised debriefing was not a regular routine, but the informants were receptive to it when it was offered. Some of the informants had not participated in an organised debriefing.
Conclusion: The informants found that situational awareness was a perception for dealing with different types of critical incidents. The study shows how a combination of organised debriefing and self-help can help registered nurses to deal with critical incidents better. It also shows that Emergency Medical Communication Centrephysicians and ambulance personnel who were present during the incident are an important resource in relation to reviews to help promote professional growth and self-assurance in work tasks. The findings help to elucidate different ways to process critical incidents after emergency calls.
Introduction
Registered nurses (RNs) working at Emergency Medical Communication Centres (EMCC) deal with multiple critical incidents of varying levels of severity when answering emergency calls.
The term ‘critical incident’ refers to an incident with a high-severity level. This has previously been defined as any incident that has resulted in, or could potentially result in, negative consequences or undesirable outcomes for patients or other people (1).
It has been shown that nurses working in EMCC experience serious and challenging incidents in their work, and the fear of making an error can result in overuse of limited resources such as ambulances (2).
It can feel challenging to perform triage and determine the degree of urgency when you cannot see the patient or the situation (2, 3). Triage is an assessment to determine the urgency and nature of the EMCCs intervention, and it entails prioritising patients on the basis of an emergency call (4).
The Norwegian regulations relating to emergency medical services require EMCCs to respond to 90% of calls within 10 seconds (5). Therefore, RNs working in EMCCs have little time to spend on individual emergency calls, which simultaneously require mental and professional preparation, good communication skills in relation to callers and colleagues, systematic collection of data and the provision of sound guidance for the caller (6). Several studies have pointed to reactions such as work-related stress, burnout and post-traumatic stress symptoms among EMCC personnel (3, 7).
Earlier research has found that RNs have a professional need to learn from their experiences and prepare for similar incidents, and a personal need to process the psychological impact and ensure that they have responded correctly (8).
A critical incident, such as a cardiac arrest with a potentially fatal outcome, can trigger powerful emotional reactions and make RNs anxious. In such cases, there will be a need for prompt reassurance that the situation has been dealt with correctly. Reassurance will help to boost confidence and is a perception for learning from experience and being able to continue working (8).
RNs working in EMCCs consistently use the Norwegian Index for Emergency Medical Assistance (Index) evaluation tool to identify, register and determine criteria for the degree of urgency when dealing with emergency calls. The Index contains several different chart sheets for emergency medical incidents, such as ‘02 Unconscious children’ (9). These tools help to ensure professional treatment and, at the same time, prepare RNs for new incidents.
Earlier research has found that knowledge (2), experience and intuition are important factors when making decisions about interventions (2, 10). It has also been found that effective practice is associated with human factors including situational awareness, decision-making, teamwork, cooperation and communication (11).
At the organisational level, it has been shown how RNs are dependent on resources in their work and support from management after critical incidents, but that resources are not always available (10).
RNs working in EMCCs may need help to process their own reactions in retrospect. Key objectives for debriefing have been described previously as learning for improvement, reducing the risk of errors and optimising treatment (11).
It has also been found that debriefing can lead to better coping skills regarding own reactions in future incidents (3, 7) and that those who have never participated in organised debriefing lack techniques that can help them to cope with their own emotional reactions (12).
By participating in debriefing, RNs also find that the development of services can occur both at the individual, team and organisation level after debriefing has been carried out (11).
Within EMD services, however, there has been little in the way of research activity concerning RNS’ perceptions of debriefing (13, 14), and its effect is poorly documented (11). Debriefing can be understood as a formal and systematic review of an entire incident in a discussion group or an individual meeting (15).
After a critical incident, RNs working in EMCCs in Norway may also participate in a technical review, which is a meeting of all of the health personnel involved in an incident. During this review, participants discuss each stage of the incident in a plenary session that allows individuals to talk about their own contributions (16).
The duty supervisor during the shift in question takes responsibility for organising the technical review. The procedure can vary according to the time and place, but the usual routine is that the review is led by the physician in charge of the incident or another health professional who was involved.
RNs working in EMCCs may also receive a telephone request to participate in an Emotional Crisis Management (Emosjonell Førstehjelp og Krisehåndtering (EFOK) debriefing, which is a Norwegian collegial support scheme that provides psychological first aid and crisis management assistance after a critical incident. EFOK is an umbrella term for psychological follow-up in a prehospital clinic. EFOK is a support measure for first responders working in EMCCs and in the ambulance service, where the facilitator leading the debriefing is employed by the prehospital clinic and has carried out certified training in collegial support (17).
There is a need for more knowledge concerning the qualities that RNs working in EMCCs may need for dealing with critical incidents, and how different measures for processing incidents are perceived as a form of retrospective support. This study will provide a basis for obtaining qualitative knowledge which will be used to develop an intervention study on debriefing later.
Objective of the study
To gain in-depth knowledge about the perceptions that RNs perceived to be required for handling with critical incidents when answering emergency calls, and their experiences of retrospective processing of incidents. The following research questions were formulated:
- What qualities do RNs working in EMCCs feel are important for coping with emotional reactions after a critical incident?
- What do RNs working in EMCCs feel about processing and debriefing in relation to their own reactions after a critical incident?
Method
The presentation of the study’s methods is based on the recommendations in the Consolidated Criteria for Reporting Qualitative Research (COREQ) (18).
Research design
The study has a qualitative design. We have conducted qualitative interviews with a grounded theory approach (GT) (19, 20), where the purpose has been to obtain qualitative in-depth knowledge regarding how RNS working in EMCCs deal with and debrief after critical incidents.
There is a need to carry out a larger survey involving more EMCCs in the future, in order to gain a more representative sample and be able to develop an intervention study on the topic based on the knowledge established.
Sample and selection strategy
The informants are RNs working in an EMCC. The selection criteria are having participated in a technical review and/or an EFOK debriefing. RNs working at one EMCC operated by a Norwegian regional health authority received a written request to participate in the study, together with an informed consent form. Age, gender, work experience and other details are not referred to to protect the anonymity of the informants.
Two informants sent a positive response within two weeks. One reason for the lack of responses was that many of those asked had not previously participated in a debriefing. Therefore, we successively recruited informants who had been through an organised debriefing later, this time based on a verbal request with reference to the information sent out earlier.
The total sample consisted of six RNs working in an EMCC. They had different experiences of organised debriefing and other ways to process a critical incident.
Data collection and data analysis
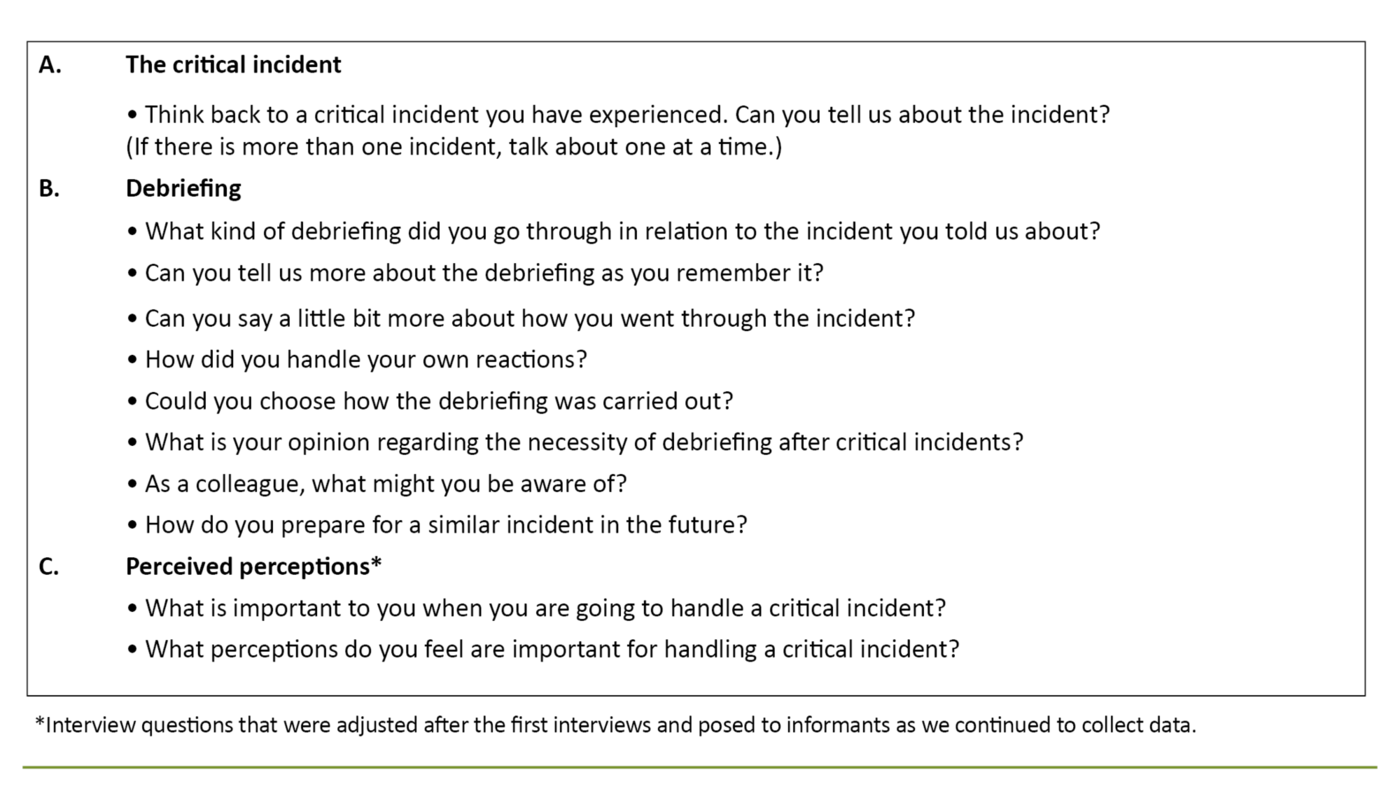
A systematic, semi-structured interview guide with themes and some overarching main questions was prepared and used in each individual interview (Table 1).
The interviews took place in the period February – July 2020 and were of 23–45 minutes duration. We conducted the first two interviews in a quiet room where we were not disturbed at the EMCC, and the later interviews were carried out over the telephone due to the outbreak of the Covid-19 pandemic.
Data collection was concluded after six interviews, as we had obtained an ample amount of data. We made audio recordings using a Dictaphone, and the audio-tapes were deleted after the interviews had been transcribed.
The interview guide was developed based on the research questions and relevant research literature on critical incidents (3, 21) and debriefing (7, 15). The interview guide was adjusted according to the data and the memos. This approach is fundamental in GT (19, 20).
Incidents and terms that had come up in the already transcribed interviews and memos were compared between informants. The information that came to light influenced the subsequent interviews, in that we adjusted some of the interview questions to confirm or discard data. For example, the perceptions that RNs working in EMCCs found necessary for coping with a critical incident was a theme that emerged from the very first interview, and this was followed up in subsequent interviews.
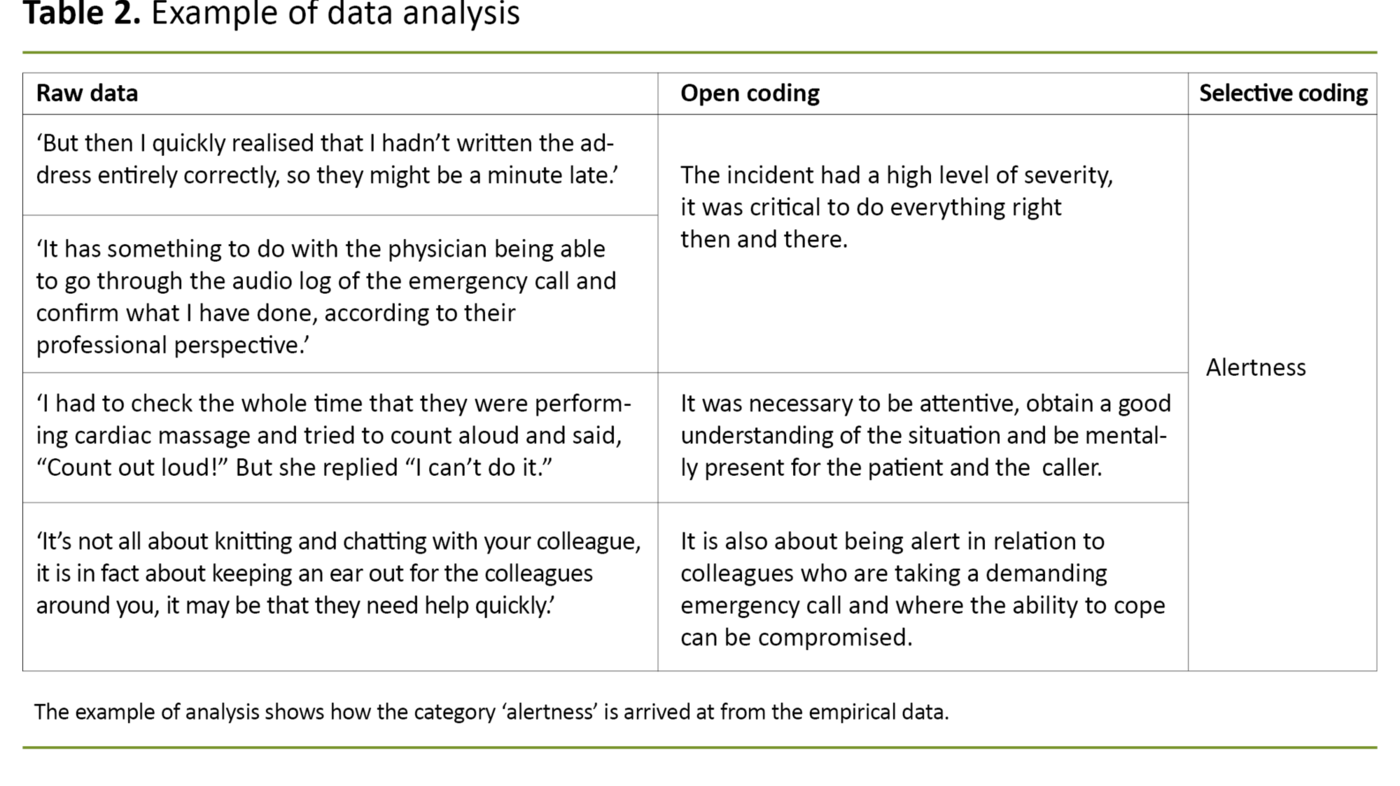
We identified various categories of perceived perceptions reported by the RNs, and the term ‘presence’ came up as a potential core category. Since the term could be understood as meaning ‘physical presence’, we searched for synonymous terms such as ‘fully attentive’, ‘attentive presence’ and ‘alertness’. The latter term was already a subcategory.
After having studied theory in the field, we became aware of the term ‘situational awareness’, which is used in a number of articles (10). This is described as an important factor for handling a critical incident.
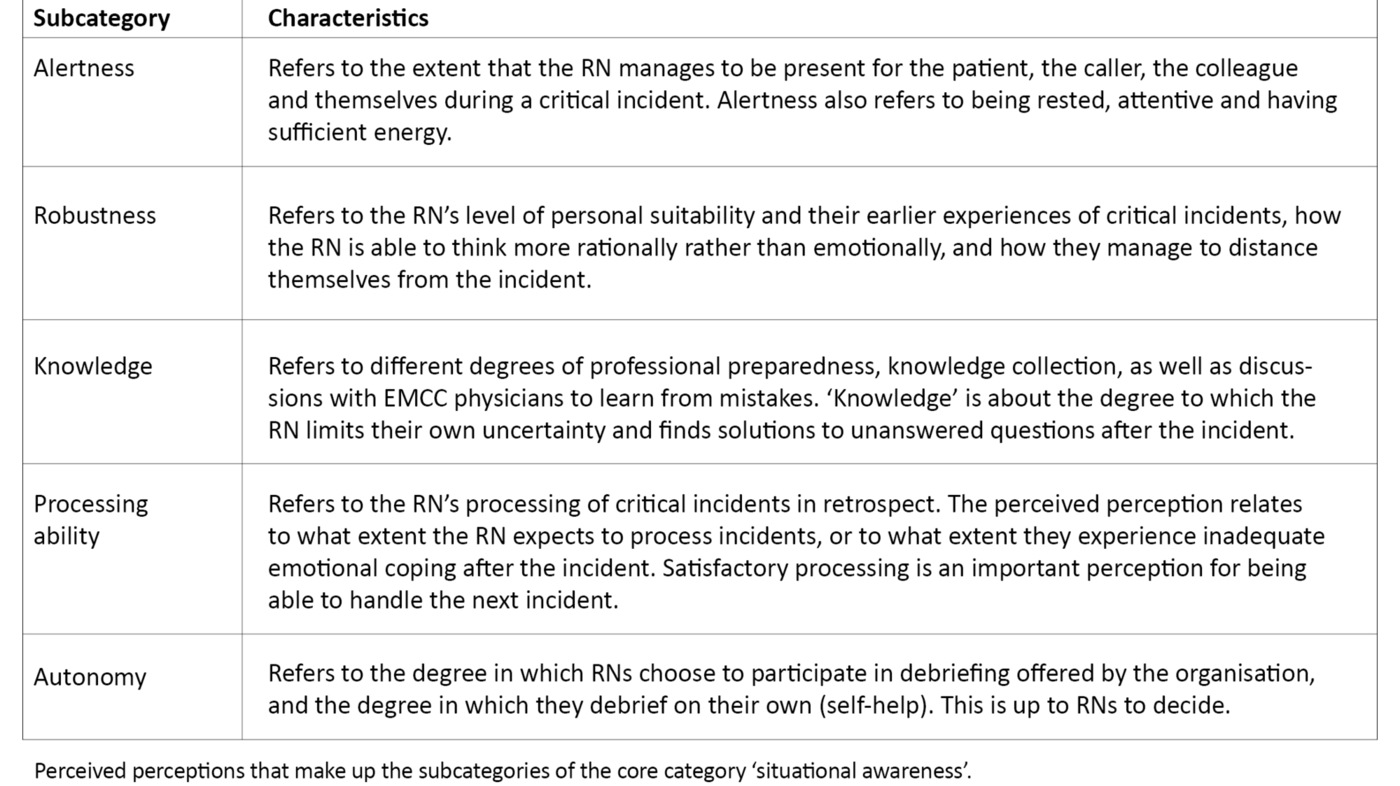
Further analysis of the data led us to choose the term ‘situational awareness’ as a core category. Related subcategories that came up in the data were ‘alertness’, ‘robustness’, ‘knowledge’, ‘processing ability’ and ‘autonomy’.
We found that there were very few RNs working in EMCCs who had experience of organised debriefing. The data indicated that several of the informants deal with their own reactions alone, without support from the organisation. The questions revealed how they performed self-help. Information in the data was compared for each informant, and the categories began to develop. In this way, data collection and data analysis were carried out in parallel.
The analysis started with an initial open coding by reading line-by-line, to become familiar with the data, followed by selective coding to identify terms that could be entered into categories. Examples of the coding process are described in Table 2.
Ethical considerations
Before the project began, the project plan was approved by the Norwegian Centre for Research Data (NSD), reference number 661110 (21). The data protection officer at the regional health authority and the managers of the EMCC had given permission to start the project. Research ethical considerations are safeguarded through informed consent after receiving oral and written information.
Participation was confirmed by signing the consent form. Everyone was informed that they could withdraw from the study at any point before the analysis commenced. After thorough consideration, it was decided that one of the managers at the EMCC should inform people about the project while being very careful not to pressure anyone to participate.
In the results section, we have decided to use some quotes, but the informants are not coded to protect their anonymity.
Results
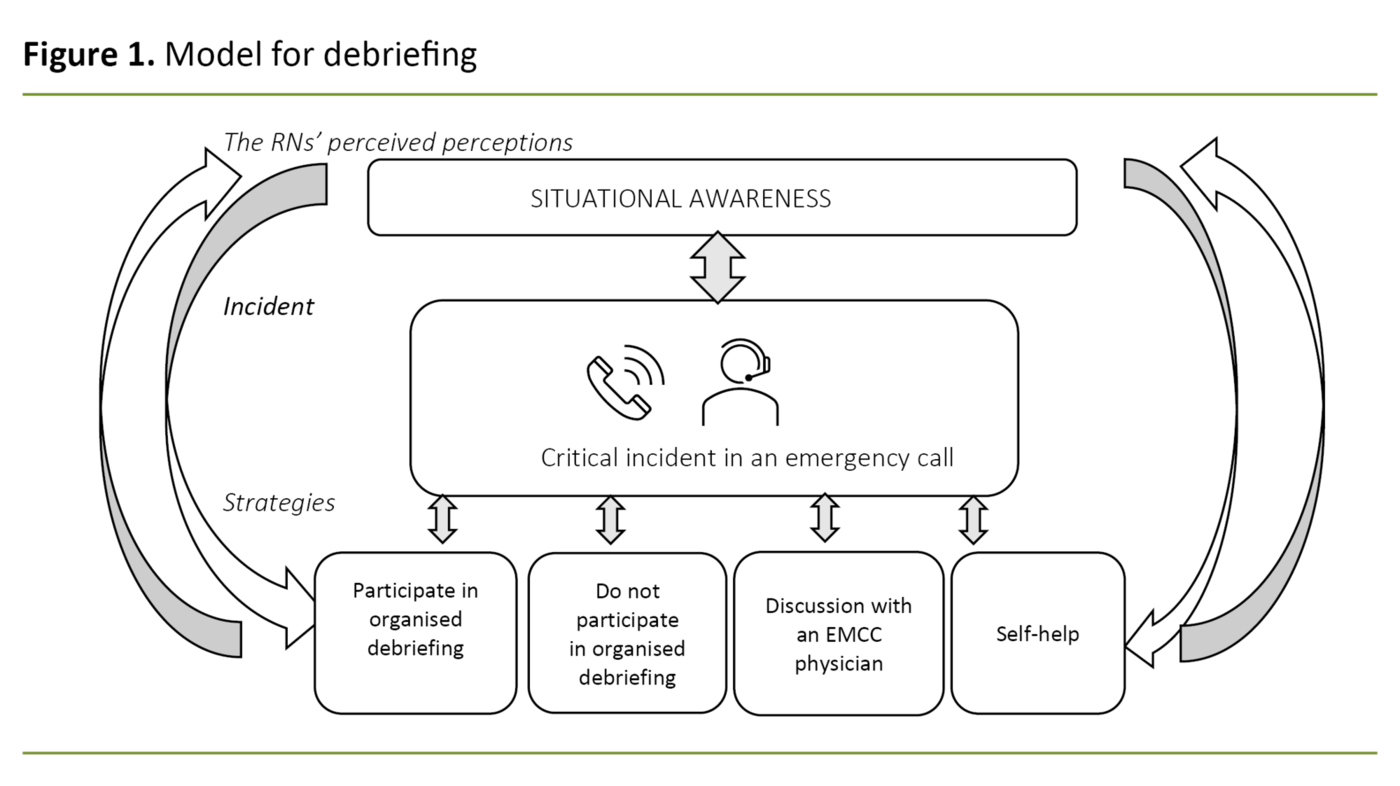
The key findings in this study indicate that the ‘situational awareness’ of RNs working in EMCCs, as well as the incident’s severity and outcome, are of significance to how they process their reactions after the event.
They either participate or do not participate in organised debriefing, seek professional support from the EMCC physicians, and/or employ measures such as self-help. The relationships between the categories are illustrated in a model (Figure 1).
RNs’ perceived perceptions for handling a critical incident
The core category ‘situational awareness’ can partially explain the background for the way that RNs working in EMCCs handle critical incidents.
Situational awareness is linked to the RNs’ attention, empathy and understanding of the situation. It is also related to the degree in which they manage to remain mentally present during a critical incident while continually monitoring the situation, including everything that happens during the conversation, the incident, as well as the organisation and the potential emergency turn-out. They must be rested and have sufficient energy. Situational awareness is linked to a fear of misjudgement, the risk of misjudgement and the risk of being reproached for the choices made. The RNs describe what they consider to be perceptions for the core category ‘situational awareness’, which are important for their choice of strategies later. These perceptions constitute the subcategories (Table 3).
They describe ‘alertness’ as the ability to be attentive, ‘robustness’ as the ability to think more rationally rather than emotionally, ‘knowledge’ as being professionally prepared using evidence-based practice, and ‘processing’ as the ability to work through their reactions to the incident. It is inherent in their perceived perceptions that they make ‘autonomous’ choices about how they do or do not debrief critical incidents in further work.
Debriefing after critical incidents
The strategies that we identified are that RNs primarily deal with critical incidents using ‘self-help’, and that they often take initiative to have a ‘discussion with the EMCC physicians or ambulance personnel. Organised debriefing is not a regular routine, and while some of the informants ‘participate in organised debriefing’, others continue to work and ‘do not participate in organised debriefing’.
‘Organised debriefing’
Few of the RNs ask to participate in organised debriefing with a technical review or EFOK, but they want to do this when it is offered and organised on the shift after very serious incidents. One RN working in an EMCC reported:
‘I think that technical reviews help to keep us secure from impressions after critical incidents. Instead of wondering whether it could have gone better or if it was my fault, I am able to work through it and clarify the incident together with colleagues. Perhaps it was not as serious as I thought.’
The informants report that it is important to receive support for their own response to and assessment of the incident, even when they feel that they are coping well with the emergency medical incident. They said that it was important to solve unanswered questions, explain their feelings in words, to be asked relevant questions, learn coping techniques and receive guidance on how to think rationally rather than emotionally, and as such get help to prevent self-reproach.
‘I had an EFOK debriefing over the telephone, which was reassuring. I didn’t attend in person. When the first conversation was over, I could relax knowing that they would call again in a week. There was nothing more I could have done.’
Some of the informants frequently find that one EFOK telephone conversation is sufficient, but sometimes several conversations are necessary to feel the benefits. This was especially the case for RNs who had dealt with serious incidents involving children.
‘No organised debriefing’
This strategy includes those who declined an offer of organised debriefing and those who did not receive an offer. RNs working in EMCCs who declined to participate, believed that they had handled the critical incident without the need for help from the organisation, but that there were other occasions on which they would have liked to have had the offer:
‘There have been times when EFOK has called where I didn’t feel the need, but there have been other occasions perhaps when I would have welcomed a call.’
Those who did not receive the offer tried, by varying degrees, to distance themselves emotionally from thinking about the incident by continuing the shift and finding the ability to cope and motivation in the subsequent emergency calls. Others pointed out that debriefing is often organised outside working hours and/or away from their place of work, and consequently they did not spend time on it as they already had a hectic daily schedule.
The informants described the ability to deal with critical incidents by being mentally present and professionally prepared. Many of them managed to handle and process emotional reactions to stressful experiences. However, the data also show that some people may have a need for debriefing immediately after an incident, but that there is not always time for this.
Another problem that can lead to inadequate emotional coping levels afterwards is that there can be many consecutive demanding emergency calls or there may be few breaks between calls for discussions with colleagues:
‘Just as I hung up the phone, I had to take the next call, so I almost didn’t have time to breathe between calls. I had to take it because it had been ringing for almost a minute, and that was how the rest of the shift was.’
‘Self-help’
Some of the RNs recalled situations that involved self-help. They prepared, for example, by improving their knowledge so that they could adapt quickly to similar incidents. Less serious incidents are often processed by taking short breaks or listening to the audio log to find errors or points for improvement.
More extensive or serious incidents are debriefed by sharing experiences from the incident with a colleague sitting close by. Some people said that it was easier to share their reactions and feelings if their colleagues had been ‘listening in’, i.e. listening to emergency calls to identify a potential need for support. However, a perception was having enough time for ‘defusing’, which is an early review of the incident to reduce the emotional trauma:
‘I’m good at talking and discussing things with someone. When I dealt with the child with a foreign object in their respiratory passage, it had been fairly quiet on the surrounding lines, so everyone had heard the call and listened in.’
At times, some of the informants prepare themselves by acquiring more knowledge, by revising or memorising special chart sheets in the Index. Some of them also applied for time off or stayed at home to recover mentally. Some informants revealed as well that they sought support from family members after ending a shift involving serious critical incidents.
‘Discussion with the EMCC physician’
After both serious and minor incidents, the RNs often turn to the EMCC physician or call ambulance personnel who were involved in the response to the incident. The purpose is to seek support, to get confirmation of their own assessment or to get an update on the specific treatment pathway in individual incidents.
They only discuss things with EMCC physicians who have the opportunity to listen to the audio log. This applies regardless of whether the RNs have been offered organised debriefing:
‘It has something to do with the physician being able to go through the call and confirm what I have done, according to their professional perspective, and I think that is an important factor in the processing.’
Discussion
A key finding in this study is that RNs working in EMCCs perceived different personal perceptions as being important for how they process incidents. The core category ‘situational awareness’ is an important perception for processing experiences after critical incidents, in which they navigate between personal and professional competence in communication with the patient, the caller and colleagues.
Several of the RNs working in EMCCs described choosing a combination of self-help and organised debriefing. Those that decline organised debriefing believe that they have a higher threshold for requesting it or they do not see the need for it and turn down the offer.
The findings also show that discussion with an EMCC physician is an important internal resource in connection with professional reviews after critical incidents. RNs often take the initiative in relation to these discussions.
Some important perceptions for handling an incident
Some important perceived perceptions for handling a critical incident are described in Table 3. They form the background for the core category ‘situational awareness’, which is an important perception for dealing with a critical incident and being able to debrief afterwards (Figure 1).
The term ‘situational awareness’ is described in research on, for example, RNs’ understanding of the situation and ability to make decisions during critical incidents (2, 22), or in connection with night shifts where alertness is most impaired due to circadian misalignment (23). The term has been used previously as an umbrella term for a range of cognitive processes or skills that include perception, understanding and anticipation (10).
Our findings are consistent with these findings, in that the RNs strive to adjust in order to be mentally present between incidents, but it can be difficult when new emergency calls are waiting to be answered. We found that the RN achieve ‘robustness’ by thinking and acting more rationally rather than emotionally.
Further, they talked about a fear of misjudgement if they did not acquire a thorough understanding of the incident, for example, that they failed to pick up obstacles that were hindering communication between the RN and the caller. Research has shown that a perception for carrying out telephone cardiopulmonary resuscitation is that the RN is supportive and observant in their contact with the caller (2).
Further, earlier research has shown how RNs attempt to create a ‘mental image’ of the incident, combined with professional knowledge of triage (24). Other research (2) describes professional preparation, the opportunity to use earlier nursing experiences, receiving support for own decisions and having more time to reflect on triage in relation to serious incidents.
The RNs in our study attempted to address unanswered questions or uncertainty after critical incidents by acquiring ‘knowledge’ through professional technical reviews with colleagues.
However, our findings show that there is a lack of uniform debriefing provided during shifts, and that RNs often make ‘autonomous’ decisions about how they deal with the incident later on. Sufficient access to debriefing during shifts can have significance for how they manage to ‘process’ an incident, something that the RNs described as an important condition for being able to deal with the next incident.
Debriefing is perceived as being important
Although the data indicates that very few people request organised debriefing, the RNs in our study find that debriefing enables them to express their feelings in words, gain clarity concerning whether they have done the right thing, and learn coping techniques so that they are able to think rationally rather than emotionally and avoid self-reproach. It is also important to talk the incident through with colleagues.
However, research shows that emergency response personnel are not always keen to be told whether they should participate in debriefing. A lack of experience in debriefing can lead to coping less well with incidents (12). Further, it is claimed that debriefing, collegial support and follow-up can be more important for the novice (25) and after serious incidents involving children (3, 22).
In our study, the RNs found that one EFOK telephone conversation was sufficient, even though there was sometimes a need for more follow-up, especially after they had dealt with an incident involving a seriously ill or injured child. But there were also cases in which the RNs did not always have a need for debriefing afterwards, where they felt that they had coped well with an emergency medical incident. There is, however, a consistent finding that RNs take the initiative to learn from specific incidents in order to be prepared, which is in line with earlier research (8).
Several of the informants had less experience with debriefing sessions in group reviews than with individual EFOK debriefings. It has previously been found that RNs experience individual debriefing differently to debriefing in groups. For example, the hierarchy in a team can create a barrier for RNs, preventing them from talking about themselves and certain other topics during debriefing (26). The hierarchy can also make it stressful to participate in such groups with colleagues.
Results like these indicate that there may be possible barriers to participation, and one should be aware that group debriefings may not always be beneficial in all situations. But research has also shown that having access to debriefing, and guidance in using this form of follow-up, can entice more people to participate, and that this can be done, for example, by sending an invitation in a text message (22).
In our research material, however, it appears that colleagues provided important support during a working day, for example, by ‘listening in’ if they had the opportunity.
Why some people decline to take part in debriefing
It has been previously shown that barriers to participating in debriefing can be created by a lack of encouragement to participate (12), uncertainty in relation to the role of a ‘debriefer’ and a lack of procedures for debriefing in an organisation (8).
Much of this is confirmed in our findings, including the observation that it is easier to decline to participate if the debriefing is held outside of working hours or away from the place of work. We also found that a technical review with colleagues was found to be just as important as a psychological debriefing, in that it provides professional reassurance and support in dealing with the incident.
Teamwork and cooperation with colleagues have also been highlighted earlier as being important in relation to critical incidents (11). It has been shown that satisfactory support from the organisation can help to reduce burnout and build resilience in those answering emergency calls (27). This is in accordance with the RNs in our study, who describe the necessity of ‘robustness’ when addressing a critical incident.
More research is called for to find strategies that are effective for overcoming barriers to debriefing, especially conveying the value and purpose of this measure to relevant health personnel (11).
Clark and McLean (8) claim that debriefing is an unexploited opportunity for RNs to learn, to get confirmation that they have done a good job and, in this way, improve their practice. Some of the RNs in our study said that they had less need for debriefing, as they feel that they can cope with emergency medical incidents. These RNs make autonomous decisions about whether or not to participate in debriefing.
With the knowledge already gained regarding the usefulness of processing and following up critical incidents, there is reason to ask whether the freedom to choose debriefing is the right way to go in the future. Perhaps debriefing and technical review should rather be established as standard practices for everyone.
Self-help and collegial support
One important finding is that self-help compensates for a lack of support in debriefing. RNs working in EMCCs described ‘processing’ as a perception for dealing with their own reactions after critical incidents. In addition, they found that short breaks, positive feedback and spontaneous discussions with colleagues about the clinical aspects of incidents with a negative outcome were all helpful.
Earlier research supports the idea that short breaks can contribute to reflection (8, 10, 28). It has also been described how the individual can benefit from immediate discussion and feedback (29), and that this form of follow-up can make RNs more self-assured. In their work. These measures are recommended for defusing, to make the situation less dramatic (10, 28, 29).
Several RNs in our study recounted defusing with their neighbouring colleague or colleagues who had ‘listened in’ after critical incidents. It was also revealed that several of the informants had the ability to distance themselves emotionally by using these sorts of self-help strategies. Furthermore, earlier research has described how the empirical knowledge of colleagues can help to promote learning in actual incidents characterised by uncertainty (25).
More time to share their own reactions is felt to be important for how they process critical incidents and seek support from colleagues on the same shift, which can also prevent stress (12, 28).
However, stress was not explicitly mentioned in our study, although several of the informants felt that they were not given the opportunity to collect themselves after a critical incident due to a large workload. But it has been shown that feedback and follow-up at work as described by our informants is linked to greater job satisfaction (26).
A professional review of the incident is also very important
A general finding is that several of the RNs seek support from EMCC physicians for a professional review. EMCC physicians’ competence and access to the audio log and the emergency call is an important internal resource in connection with professional reviews of concrete individual incidents. This type of consultation is linked to promoting positive learning experiences (8, 10).
This finding may indicate that EMCC physicians can provide a review that is just as important as an EFOK consultation, where the ‘debriefer’ is not necessarily as familiar with the content of emergency calls.
The RNs in our study stressed that ‘knowledge’ was a perception for being prepared for a situation and learning for the next incident. At the same time, they discuss good practices and areas for improvement in practice both at an individual and a team level, something which is emphasised as important in earlier research on debriefing (11, 25).
A professional review and discussion are also important to address the RNs’ uncertainty after an incident and reassure them that they have done the right thing, even if, for example, an attempt at resuscitation was unsuccessful.‘Knowledge’ is a finding that is supported by other research that shows that RNs’ professional need to learn from experience and prepare for similar incidents is also a part of processing the psychological impact of being involved in a serious incident (8). The professional review is therefore very important for RNs working in EMCCs and will form part of a future model for debriefing.
Strengths and weaknesses of the study
The study has generated new and significant knowledge on the debriefing of RNs after critical incidents at an EMCC in Norway. The first author is an RN who works at the EMCC where the study was conducted and can therefore be described as an insider, i.e. the researcher has previous knowledge and understanding about the field of practice and the issues being studied (30).
Although it can be perceived as a disadvantage to have a possible bias, it is an advantage to have ready access to the field. Communication with the informants is more effective if you have competence and personal experience related to the topic in question.
Using one of the managers to convey the request to participate could also be questioned; in this sense, it is possible to say that there was a power disparity between the person making the request and those who received it. We assumed it would be more difficult for them to decline as colleagues of the first author than it would be to a manager who you can usually discuss problematic issues with.
Another challenge was that the selection criteria proved to be difficult to meet, as not all of the RNs had participated in organised debriefing as we had previously assumed. Therefore, we changed the inclusion criteria under way, so that we could successively ask those who participated in organised debriefing later.
None of the informants withdrew after the inclusion criteria were changed, and the basis for data saturation was improved through a theoretical selection as described in GT (20), since we gradually included informants who had participated in organised debriefing.
The study has a small sample size, but the data provides guidance for a future, larger study in that we discovered that very few informants had participated in organised debriefing and that they chose different strategies to process and debrief after incidents.
The findings are not transferable to other EMCCs, but they may be of general interest nevertheless. The study’s findings may also be relevant to RNs working at an out-of-hours medical service in Norway, as they often interact with EMCCs in the case of serious incidents.
Therefore, there is a need for further research with a larger sample, in which a greater number of EMCCs can be surveyed to examine representativeness and follow-up by debriefing at EMCCs in general.
We also found that a complaint after an incident is often the cause of considerable stress to RNs and is a type of critical incident, but this topic is not addressed in this article. Complaints can be considered as a general problem in which RNs and other personnel may also need following-up afterwards.
Conclusion
This study has shown that RNs working in EMCCs handle their own reactions after critical incidents using both self-help and collegial help, together with conversation with EMCC physicians and the acquisition of more knowledge. Situational awareness is an important perception for handling a critical incident. The fact that only some of the RNs had received an offer of organised debriefing (EFOK), and only after some critical incidents, shows that this form of debriefing is not part of the routine at the EMCC that was examined.
The study does not provide answers regarding other EMCCs in Norway, but the findings are in accordance with earlier research. Therefore, there is a need for further research in this area of emergency medical treatment. Intervention studies will be particularly valuable to contribute to more knowledge in this area. Such studies can also contribute to protecting RNs in relation to their emotional reactions after critical incidents.
The authors declare no conflicts of interest.















Comments